Are Your Symptoms Thyroid or Perimenopause Related?

In the early stage of the perimenopause transition, symptoms can be confusing for many women. Add the potential for thyroid issues, and confusion increases along with added health concerns. Are those extra pounds related to aging or hypothyroidism? Is perimenopause responsible for your mood swings and increased fatigue, or is it something else?
Read on to learn how the thyroid works and why it matters for good health, and why perimenopause symptoms can be so easily confused with thyroid conditions. We include tips on natural treatments you can practice assuring your thyroid is balanced, protecting your overall well-being.
Thyroid Function and Women
Thyroid disease affects over 12 percent of the U.S. population. Over half of people do not know they have a thyroid condition. Women experience thyroid conditions several times more than do men, with one female in eight being affected. Incidence increases beginning at 35 years, with prevalence growing to 20% among women over 65.
The thyroid is located at the front of the neck, with its butterfly shape wrapping around your windpipe (trachea). It secretes hormones that manage many critical body functions, including heart rate, temperature, metabolism, menstrual cycles, and more. The two main hormones produced by the thyroid are commonly known as T3 and T4. TSH is the thyroid-stimulating hormone produced in the pituitary gland; it regulates our body’s T3 and T4 levels. When our T3 and T4 hormones are too high or low, they can create symptoms that mimic perimenopause, affecting our sensations of heat or cold, weight gain, or (more rarely) loss, mood, and digestion. There are many triggers for thyroid disease, among them nutrient deficiencies, fluoride and heavy metal toxicity, a major illness or virus, pregnancy and childbirth, and stress.

Are These Perimenopause or Thyroid Symptoms?
Estrogen production becomes more erratic with the onset of the menopause transition, which can begin as early as one’s 30s, with changes in monthly cycles typically becoming noticeable during our 40s. Perimenopause duration varies from one woman to the next, extending for months or years. It comes with an array of symptoms, from night sweats to changes in menstrual cycle frequency and character. Shifting hormone levels, especially estrogen, are responsible for mood swings, foggy thinking, and waves of hot flashes. Added to that are sleep disruptions and the discomfort of vaginal dryness.
The ups and downs in estrogen that occur during the menopause transition influence thyroid function because estrogen regulates the hormone-binding protein, thyroid-binding globulin (TBG). When estrogen levels are high, the liver produces more TBG. Thus the amount of T3 and T4 that are available in the bloodstream temporarily drops until the thyroid gland is stimulated to produce more. Conversely, when estrogen levels temporarily drop, during a skipped menstrual cycle, for example, TBG levels drop, and the amount of ‘free’ T3 and T4 increases temporarily. These shifts in thyroid hormones are not well understood but may influence some of the symptoms that women experience during perimenopause.
For some women, weight gain and irritability may be an indication of thyroid issues. The question becomes: How does a woman know if her symptoms are related to perimenopause or due to a thyroid condition?
Perimenopause or Thyroid Problem?
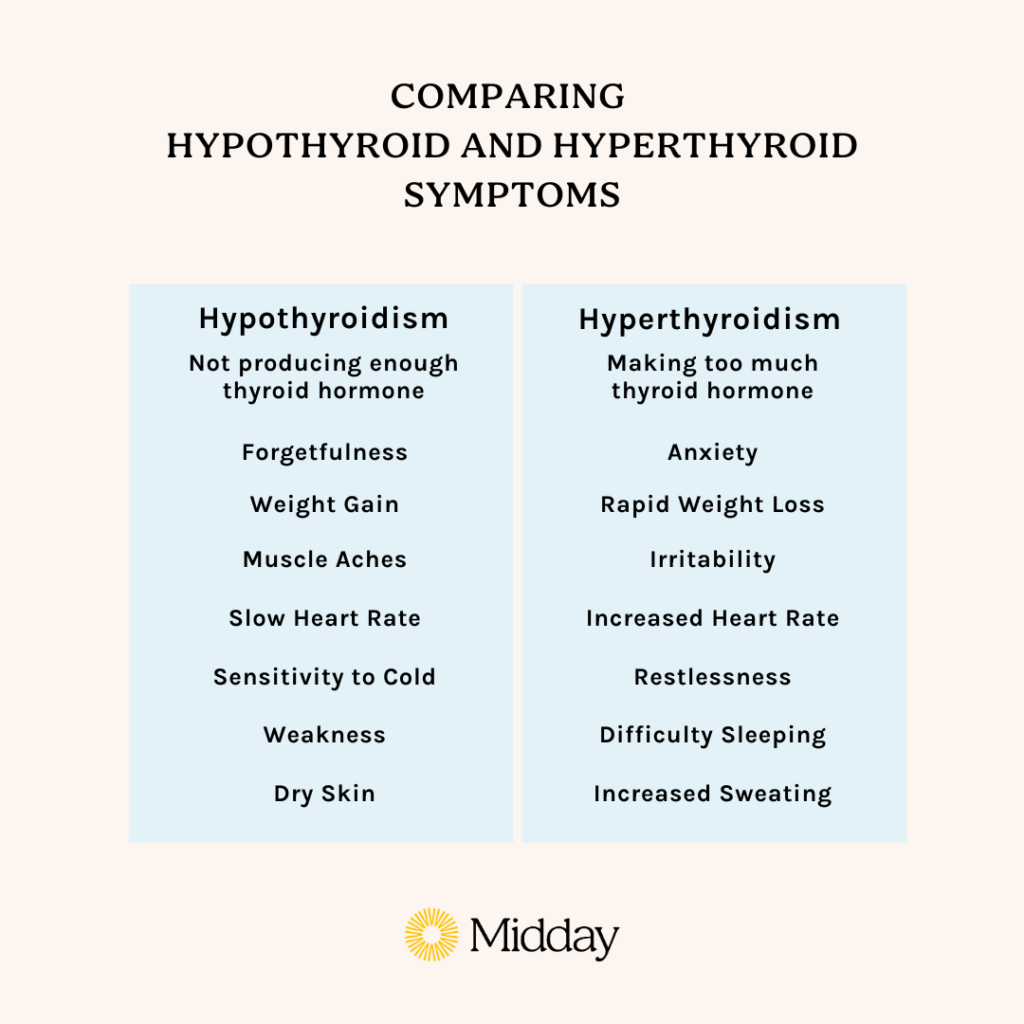
To answer that, let’s discuss what happens when the thyroid secretes too little, or too much, of its T3 and T4 hormones. Hypothyroidism is a good place to start, as its symptoms often overlap with female midlife changes.
Hypothyroidism
When the body’s thyroid levels fall below normal ranges, many bodily functions slow. A person fatigues more readily than in the past, skin becomes drier, and constipation can develop. A woman may notice she’s feeling down more often, her memory stalls, and her once dependable menstrual cycles change. She may feel cold all the time.
Hypothyroidism is most often associated with autoimmunity. Hashimoto’s is the most prevalent cause of hypothyroidism. Hashimoto’s disease is a condition in which your immune system attacks your thyroid. An enlarged thyroid, called a goiter, may appear, which may make the front of your neck look swollen. If you have another autoimmune condition or Hashimoto’s runs in your family, your risk of having the condition is higher.
Hypothyroidism may be underdiagnosed if its symptoms are attributed to perimenopause without appropriate testing. Testing guidelines are somewhat controversial, and there is no uniform agreement about the best interval for testing. Many clinical guidelines recommend screening women’s TSH level beginning at age 40 and every five years after that. Women with symptoms of menopause or perimenopause should have a thyroid screening test performed if one was not done recently to assure that a thyroid problem is ruled out.
It’s very important to discuss your concerns with your primary care provider (PCP) as hypothyroidism that goes untreated contributes to elevated cholesterol, blood pressure, the risk of heart disease, and other conditions. Fortunately, it is diagnosed with a simple blood test and can be easily treated with a medication called levothyroxine.
You can also improve your thyroid function with natural remedies that may allow you to reduce the dose of your prescription medication or discontinue it altogether.
10 Holistic Practices to Improve Thyroid Health
Try to incorporate these dietary and lifestyle changes into your life to prevent problems with your thyroid:
- Eat a healthy diet with a wide variety of plants.
- Get adequate iodine from sea vegetables, iodized salt, fish, and eggs (Note: natural sea salt does not contain iodine).
- Include more foods containing selenium, such as Brazil nuts, spinach, and tuna.
- Avoid frequent consumption of cruciferous vegetables, particularly when raw.
- Eliminate inflammatory foods like gluten, refined sugars, and dairy.
- Add in gut-healing foods rich in prebiotics and probiotics.
- Improve your sleep to reduce your body’s stress load.
- Get plenty of exercise to maintain a healthy weight.
- Reduce your stress level.
- Review medications and supplements with your healthcare provider, as some may interfere with the body’s absorption of thyroid hormone.
After you’ve followed these lifestyle modifications for a period of time, speak with your doctor about reevaluating your thyroid function and prescription medication. Never make adjustments to your medication without consulting your doctor first.
Although there is no cure, medication, lifestyle changes, and consistent monitoring can make a person feel more like herself!

Hyperthyroidism
Less common than hypothyroidism, hyperthyroidism, the overproduction of thyroid hormones, can also mimic perimenopause! Just think of these issues compared with menopausal symptoms you read about:
- Irritability and trouble sleeping,
- Sweating a lot and feeling uncomfortable when warm,
- Palpitations,
- Menstrual flow lightens, and cycles are less frequent, and
- Bursts of energy shift to becoming easily fatigued.
Other symptoms include diarrhea, heavy menstrual periods, high blood pressure, and weight loss despite having an increased appetite.
These are signs to discuss with your PCP, especially because an over-active thyroid adds risks for health complications such as osteoporosis and cardiovascular disease.
Hyperthyroidism is diagnosed by examination and simple blood work. It’s usually caused by a different kind of autoimmune disease called Graves’ disease. You may be referred to an endocrinologist, a specialist in the endocrine system, including glands and the hormones they make, as treatment options vary depending on the diagnosis.
There is no natural cure for hyperthyroidism. However, dietary changes can help manage symptoms.
- Avoid foods high in iodine, including iodized salt, cheese, milk, eggs, saltwater fish, and junk and processed foods.
- Avoid foods and beverages high in caffeine as they can worsen symptoms.
- Eat a healthy, balanced diet, including vegetables and lean protein.
- Include more foods containing selenium, such as Brazil nuts, spinach, and tuna.
- Maintain adequate amounts of iron by eating foods like sardines, spinach, chickpeas, and lentils.
- Boost your bone health with non-diary calcium-rich foods, including sardines, kale, and broccoli, as dairy products contain iodine.
The Benefits of Thyroid Health
The main benefit of having a healthy thyroid is the regulation of our metabolism. This becomes especially important as we age, our metabolism starts to slow, and the pounds creep on. A healthy thyroid can help keep your metabolism under control and avoid disruptive symptoms and health risks.
If you are experiencing any of the symptoms described, visit your physician and discuss your concerns. A clear understanding of what’s going on with your body will give you peace of mind and empower you with the knowledge of how to manage your symptoms best and restore your well-being. If your physician dismisses your symptoms or your symptoms persist despite making lifestyle changes, find another physician specializing in menopausal care or ask for a referral to an endocrinologist. Whether it’s perimenopause or a thyroid issue, you deserve to be listened to and to get to the bottom of your symptoms.
For more insights into where you may be at in your perimenopause journey and information on symptoms, download Midday from the App Store or visit us at Midday.Health.
Dr. Nanette Santoro is a leading clinician and researcher in Reproductive Endocrinology. She is currently Professor and E Stewart Taylor Chair of Obstetrics & Gynecology at the University of Colorado School of Medicine. She also directed the Division of Reproductive Endocrinology at two medical schools: New Jersey Medical School and the Albert Einstein College of Medicine. She is the author of over 120 scientific publications and two books. Dr. Santoro’s major research interests include the reproductive endocrinology of premature, peri-, and postmenopause, infertility, and the physiology of gonadotropin-releasing hormone secretion. She has been involved with numerous large-scale industry- and government-supported clinical trials, including the Study of Women’s Health Across the Nation (SWAN), the Kronos Early Estrogen Prevention Study (KEEPS), and the Reproductive Physiology of Ovarian Failure, and is a co-editor of the Textbook of Perimenopausal Gynecology. Dr. Santoro received her medical degree at Albany Medical College and completed her residency at Beth Israel Medical Center and fellowship at Massachusetts General Hospital, Harvard Medical School.
Sign up for more unique women’s health content
By submitting this form, you agree to the Lisa Health Privacy Policy and Terms of Use


