How to Tell What Stage of Menopause You’re In

Are you unsure what stage of menopause you’re in – premenopause, perimenopause, or postmenopause? Don’t worry, many women are confused by the terminology and how to tell when they have transitioned from one stage to another. When asked about their menopausal status, women usually say that they are “in menopause” without knowing the specific stage they’re in, how long it will last, and what to expect. Our guide to the stages of menopause removes the complexity and mystery surrounding this pivotal phase of a woman’s life.
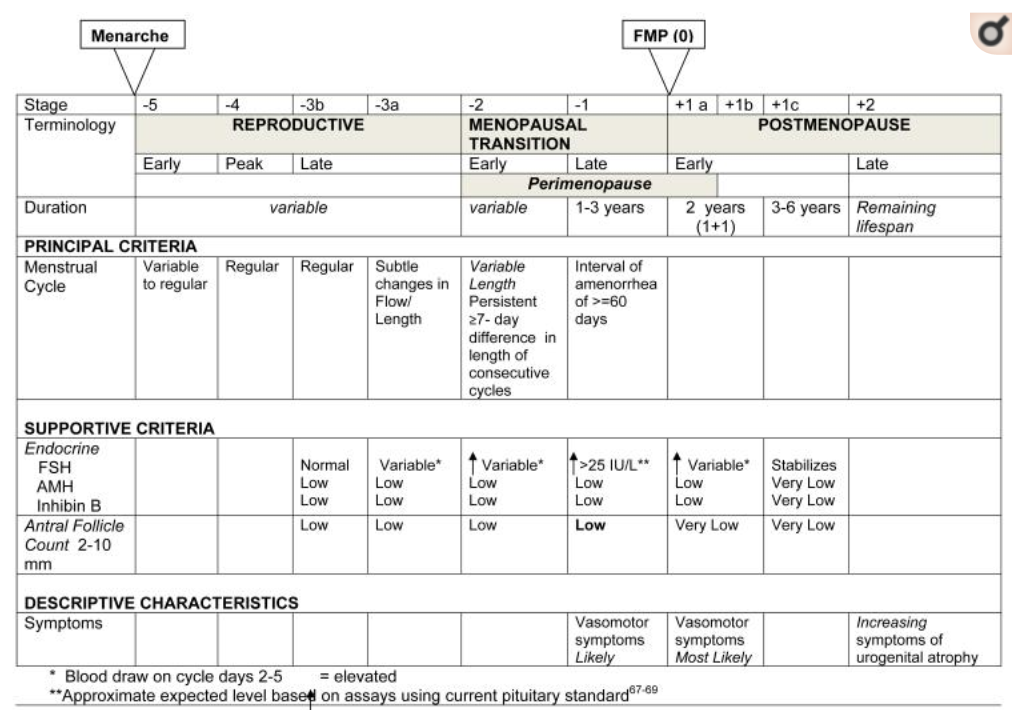
Let’s Start With STRAW
You might be wondering what the heck STRAW is. STRAW stands for Stages of Reproductive Aging Workshop. In 2001, scientists devised a standardized staging system and terminology for ovarian aging, including menstrual and qualitative hormonal criteria to define each stage. One of the drawbacks of the original STRAW system is that it could only be applied to what was considered “healthy” women. Fast forward to 2011. With advancements in knowledge, scientists gathered together again and updated and simplified the criteria, calling it STRAW+10. The STRAW+10 staging system is applicable to all women regardless of age, demographic, body mass index, or lifestyle characteristics. The STRAW criteria are widely considered the gold standard for characterizing reproductive aging through menopause.
Don’t worry, there won’t be a test on STRAW later! The background on STRAW is helpful to understand that the method for determining your menopause stage and terminology has consensus from leading menopause experts around the world and is used widely in clinical practice.
The Three Stages Of Menopause
Premenopause
When you are in your reproductive years and have regular periods, you are considered premenopausal. Your reproductive capacity starts to peak around age 30 and begins to decline sharply around age 35. In your late 30’s, there may be very subtle changes in your menstrual flow and length. You usually don’t experience any symptoms of menopause.
A small percentage of women experience menopause symptoms in their mid to late 30’s. However, it isn’t until their early to mid 40’s that most women start to notice symptoms of perimenopause.
About 1.1% of women will undergo premature menopause before age 40. Causes of premature menopause include cancer treatment, surgical removal of the ovaries, and Primary Ovarian Insufficiency. Symptoms you may experience include: irregular periods, mood swings, vaginal dryness, pain during sex, hot flashes and night sweats, low libido, sleep disturbance, weight gain, and changes in cognition and memory. If you experience any of these symptoms, it’s best to consult your physician to rule out causes other than premature menopause and discuss treatment options.

Perimenopause
Perimenopause, the transition to menopause, is broken down into two substages: early perimenopause and late perimenopause.
Early Perimenopause
During early perimenopause, you will notice changes in the length of your menstrual cycle of more than seven days. It helps to start tracking your period if you are not already doing so. This first phase of menstrual cycle change can last for several years. Early perimenopause symptoms are subtle for most women. In fact, many women confuse menopause symptoms like sleep disturbance and fatigue with other things like simply being tired or stressed from work or home life, and don’t realize they’ve started the menopause transition.

Late Perimenopause
When women enter the later phase of perimenopause, they usually begin to suspect that they are in perimenopause. The signs become much more clear. For example, your period will become noticeably irregular. You’ll start skipping periods and going a month or two at a time without a period. Your flow may change as well. Despite these changes and your age, it’s important to realize that you can still get pregnant and should continue to take precautions to prevent an unwanted pregnancy.
In addition to menstrual cycle changes, menopause symptoms become much more noticeable for most women. It’s around this time that hot flashes and night sweats usually make their appearance, along with other typical signs like trouble falling asleep or staying asleep, fatigue, vaginal dryness, lack of interest in sex, and moodiness. It’s worth noting that about fifteen percent of women have no perimenopause symptoms, and about fifteen percent of women have very severe symptoms. The rest of us are somewhere in the middle, finding that symptoms are mild to moderately disruptive to our quality of life and well-being.
Sleep disturbance is a particularly common problem and warrants more discussion. Up to sixty percent of women in the menopause transition experience difficulties sleeping. Unfortunately, sleep disturbance may only get worse in postmenopause. Many women ignore poor sleep, relying on caffeine and sheer will to make it through their day. However, sleep disturbance should not go ignored. Poor sleep and chronic insomnia are linked to a host of serious health issues, including a higher risk of depression, obesity, poor immune system function, difficulties with concentration and memory, and more. It’s well worth addressing this symptom early and investing time in improving your sleep hygiene.
When you are in late perimenopause, the expert’s best estimate is that you will reach menopause in one to three years. This is a good time to talk to your doctor about what you’re experiencing. Any changes in your menstrual cycle should be reported, especially if you have heavy bleeding.
Postmenopause
Most women reach menopause naturally between the ages of 40 and 58, with 51 being the average age at menopause. When a woman reaches menopause between the ages of 40 and 44, it’s called early natural menopause. About five percent of women have early natural menopause. Another five percent of women fall into the late natural menopause category. Meaning they’ve reached menopause after age 55.
What causes a woman to reach menopause early or late? Lifestyle factors like smoking, chemotherapy or radiation, and surgical removal of the ovaries are the most common causes of early natural menopause. Lifestyle factors and obesity are the typical reasons for reaching menopause late.
What do we mean by “reach” menopause? Reaching menopause naturally is defined as going twelve consecutive months without a period. If you go eleven months without a period and then have a period, the clock starts over. You must have gone twelve months in a row without a period to have transitioned from perimenopause to postmenopause. Once you reach this milestone, you are officially postmenopausal and will be for the remainder of your life. There is no reason to confirm your postmenopause status, but your physician can order a test under certain circumstances.
Like perimenopause, scientists now recognize that there are two substages to postmenopause – early and late.
Early Postmenopause
Early postmenopause lasts about five to seven years. Hot flashes and night sweats are quite common in this stage, with up to sixty to eighty percent of women reporting this symptom. Like hot flashes and night sweats, the perimenopause symptoms mentioned in the previous section may become more frequent and intense. In total, there are thirty-four possible menopause symptoms in innumerable combinations, making each woman’s menopause experience unique.
There are different strategies for managing symptoms, including various FDA-approved pharmaceutical options, lifestyle modifications, and a combination of the two. Most physicians recommend that you try making lifestyle adjustments for six months to see what impact they have on your symptoms. Many symptoms respond well to changes in diet, exercise, and mind-body strategies like meditation and yoga.
It’s important to recognize that you don’t need to suffer in silence or shame, particularly if you are experiencing depression, anxiety, mood swings, or other mental health issues. Depression and anxiety are common during menopause, and many women are underdiagnosed. Please seek help from a qualified physician or therapist to help you deal with these issues.

Late Postmenopause
In late postmenopause, you may find that most of your symptoms start to decrease in intensity and frequency or go away altogether. The exception is genitourinary symptoms (officially known as Genitourinary Syndrome of Menopause (GSM) which usually become more severe for about fifty percent of women. These include vaginal atrophy, which is thinning, drying, and inflammation of the vaginal walls that may occur when your body has less estrogen. Vaginal atrophy can make sex more painful and can lead to other urinary issues. The good news is that there are many options for treating vaginal atrophy, including simple over-the-counter remedies that are easy to use. There are also low-dose local vaginal estrogen and other therapies that are safe and effective. Unfortunately, very few women bring this topic up with their provider, perhaps out of embarrassment. However, healthcare providers are used to discussing intimate matters every day, so you shouldn’t hesitate to share your concerns. Women who have an active sex life as they age report better quality of life and relationships.
Your Best Chapter
While we talked about the various menopause stages and substages in a very science-y way, menopause, taken as a whole, should be viewed as a life stage. One that every woman will experience and that lasts about one-third of our lives. Many women find that the menopause life stage is the most liberating and rewarding of their lives. They find freedom, empowerment, creativity, wisdom, and other superpowers they didn’t know they had. While the uncertainty around the changes that are happening with your body can be disconcerting, to say the least, knowledge is power, and with power comes control. Taking a positive view of menopause and approaching this life stage with confidence, optimism, and enthusiasm can make a major difference in your physical and mental well-being. Don’t wait for your superpowers to find you. Discover your superpowers with all the focus and passion you can muster!
If you are still unsure about what stage of menopause you are in, here are a few resources to help you find out:
- Download Midday from the App Store and use our science-backed tool to get insights into what stage of menopause you’re in and track your menopause progression from one stage to the next, so you know what’s coming next.
- Talk to your healthcare provider.
- If your provider doesn’t seem knowledgeable or is dismissive of your questions, search the North American Menopause Society’s database for a certified menopause practitioner (NCMP) in your area. You deserve to have a healthcare provider that understands this complex and challenging period in your life and can support you to feel your best every day.
Dr. Risa Kagan, MD, FACOG, CCD, NCMP is a leading clinician and researcher in Gynecology and Menopause. She is a board-certified obstetrician-gynecologist at Sutter Health and has been a Clinical Professor in the Department of Obstetrics, Gynecology, and Reproductive Sciences, University of California, San Francisco for over 35 years. She is a North American Menopause Society (NAMS) Certified Menopause Practitioner (NCMP) and is certified by the International Society of Clinical Densitometry (CCD). She was previously co-medical director and principal investigator (PI) for multiple clinical trials at the Foundation for Osteoporosis Research and Education (FORE) in Oakland, CA, and now serves on the Medical and Scientific Advisory Board of American Bone Health (ABH). She is also a PI on numerous women’s health clinical research trials with the Jordan Research and Education Institute (REDI) of the Alta Bates Summit Medical Center, Sutter Health Research Institute. Dr. Kagan is the author or co-author of numerous publications in peer-reviewed journals and is on the editorial board of Menopause. She is often an ad hoc reviewer for many other journals including The Journal of Women’s Health and The Journal of Sexual Medicine. She specializes in gynecology with particular focus on gynecologic surgery and women’s health issues including menopause, bone health, female sexuality, and female cancer survivorship. Dr. Kagan is regarded as one of the leading physicians in her field and has been nationally listed in US Best Doctors for many years. Dr. Kagan graduated from New York University and the Albany Medical College of Union University. She completed her internship-residency at the University of California San Francisco.
Sign up for more unique women’s health content
By submitting this form, you agree to the Lisa Health Privacy Policy and Terms of Use


